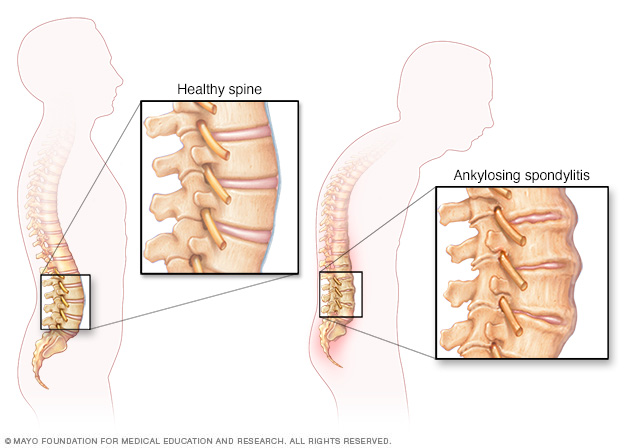
- Ankylosing spondylitis is a form of arthritis that is long-lasting (chronic) and most often affects the spine .
- It can cause pain, stiffness, swelling, and limited motion in the low back, middle back, and neck, and sometimes areas such as the jaw, shoulders, hips, knees, and heels.
- Ankylosing spondylitis is more common in men than women.
CLINICAL MANIFESTATIONS:
- Inflammation primarily of the joints of the spine, but it can also involve inflammation of the eye, other joints (especially the hips)
- on occasion, the heart, lungs, and chest wall. If the inflammation continues over time, it will lead to scarring and permanent damage.
- In some people, the disease is mild and progresses slowly, and symptoms never become severe. Other people may have a more aggressive disease process.
PATHOPHYSIOLOGY:

- Ankylosing spondylitis (AS) is a systemic rheumatic disease,meaning it affects the entire body. Approximately 90% of people with AS express the HLA-B27 genotype, meaning there is a strong genetic association. 1-2% of individuals with the HLA-B27 genotype contract the disease.
- Tumor necrosis factor-alpha (TNF a) and IL-1 are also implicated in ankylosing spondylitis. Autoantibodies specific for AS have not been identified. Anti-neutrophil cytoplasmic antibodies (ANCAs) are associated with AS, but do not correlate with disease severity.
- The association of AS with HLA-B27 suggests the condition involves CD8 T cells, which interact with HLA-B.This interaction is not proven to involve a self-antigen, and at least in the related reactive arthritis, which follows infections, the antigens involved are likely to be derived from intracellular microorganisms.
- There is, however, a possibility that CD4+ T lymphocytes are involved in an aberrant way, since HLA-B27 appears to have a number of unusual properties, including possibly an ability to interact with T cell receptors in association with CD4 (usually CD8+ cytotoxic T cell with HLAB antigen as it is a MHC class 1 antigen).
- “Bamboo spine” develops when the outer fibers of the fibrous ring (annulus fibrosus disci intervertebralis) of the intervertebral discs ossify, which results in the formation of marginal syndesmophytes between adjoining vertebrae.
SIGNS AND SYMPTOMS:
- Pain and stiffnes: Constant pain and stiffness in the low back, buttocks, and hips that continue for more than three months. Spondylitis often starts around the sacroiliac joints, where the sacrum (the lowest major part of the spine) joins the ilium bone of the pelvis in the lower back region.
- Bony fusion: Ankylosing spondylitis can cause an overgrowth of the bones, which may lead to abnormal joining of bones, called “bony fusion.” Fusion affecting bones of the neck, back, or hips may impair a person’s ability to perform routine activities. Fusion of the ribs to the spine or breastbone may limit a person’s ability to expand his or her chest when taking a deep breath.
- Pain in ligaments and tendons: Spondylitis also may affect some of the ligaments and tendons that attach to bones. Tendonitis (inflammation of the tendon) may cause pain and stiffness in the area behind or beneath the heel, such as the Achilles tendon at the back of the ankle.
- Ankylosing spondylitis is a systemic disease, which means symptoms may not be limited to the joints. People with the condition also may have fever, fatigue, and loss of appetite.
- Eyeinflammation (redness and pain) occurs in some people with spondylitis. In rare cases, lung and heart problems also may develop.
- Tenderness at the heel.
- Pain and swelling in a finger or toe.
- Tendernsess at the base of your pelvis.
- Chest pain.
- Inflammation of the eyes.
- Inflammation of the bowel.
- Tirdness(Fatigue).
MILD OR EARLY ANKYLOSING SPONDYLITIS:
- Usually starts with dull pain in the low back and back stiffness. Some people have “flares” of increased pain and stiffness that may last for several weeks before decreasing again.
- Affected bones of the low back, middle back, hips, or neck may become painful, stiff, and limited in motion. Pain tends to increase slowly over a period of weeks or months, and it is often hard to point to exactly where the pain is. Stiffness is usually worse in the morning. Physical activity often helps decrease pain and stiffness.
- A feeling of tiredness is common as the disease progresses. This tiredness comes from the body fighting the inflammatory process that is part of ankylosing spondylitis, and from ongoing stiffness and pain.
- The colored part of the eye (iris) may become inflamed. This inflammation, called iritis, occurs in about 25% to 30% of people with ankylosing spondylitis.Symptoms of iritis include redness and pain in the eye and sensitivity to light.
SEVERE OR ADVANCED ANKYLOSING SPONDYLITIS:
- Scarring in the spine causes the joints of the spine to grow together (fuse, or “ankylose”). As the bones fuse , back pain will gradually go away, but the spine will remain very stiff and unable to bend. The fused spine is more likely to break.
- The upper spine can curve forward until eventually the person has a hard time looking straight ahead. In addition, as the spine loses its natural curves it becomes hard to balance for standing and walking, especially if the hips are also affected.
- Breathing can become difficult as the upper body curves forward and the chest wall stiffens. Severe ankylosing spondylitis can also cause scarring of the lungs (pulmonary fibrosis) and an increased risk of lung infection. This can cause even greater problems in smokers because their lungs are already more prone to lung infection and scarring.
- Scarring in the eye can lead to permanent visual impairment and glaucoma.
- In rare cases, the heart muscle can become scarred and the heart valves may become inflamed. The heart may be unable to pump properly (heart failure). The main artery leading from the heart (aorta) can also be affected by becoming inflamed and enlarged near where it leaves the heart.
DIAGNOSTIC TEST:
- X-rays of the spine and pelvis to check for bone changes (bony erosions, fusion, or calcification of the spine and sacroiliac joints). Certain changes in the sacroiliac joint confirm the diagnosis of ankylosing spondylitis, but those changes can take several years to develop enough to show on X-ray.
- MRI and ultrasound are both being studied as ways to diagnose ankylosing spondylitis earlier.
- A genetic test (through a blood test), which may be done to determine the presence of a particular gene (HLA-B27) that is often associated with ankylosing spondylitis. This test will not confirm whether you have ankylosing spondylitis. However, if you have the HLA-B27 gene, you could pass it along to your children. This would increase the chances they could get ankylosing spondylitis or one of the other spondyloarthropathies.
You will have a physical exam to see how stiff your back is and whether you can expand your chest normally. Your doctor will also look for tender areas, especially over the points of the spine, the pelvis, the areas where your ribs join your breastbone, and your heels.
INTERVENTION/ TEACHING:
- Reducing pain by taking pain relievers such as nonsteroidal anti-inflammatory drugs, or using heat to decrease your pain and stiffness.
- Warm showers or baths or sleeping under a warm electric blanket may reduce stiffness.
- Exercising regularly. This reduces pain and stiffness and helps maintain fitness and mobility of the spine, chest, and joints.
- Deep breathing exercises can improve or maintain lung capacity.
- Swimming as part of your exercise program helps to maintain chest expansion and movement of the spine without jarring the spine. Breast stroke is especially good for chest expansion.
- You should avoid contact sports, since joint fusion may make your spine more likely to fracture as the disease progresses, but your doctor may approve of other activities such as golf and tennis.
- Maintaining proper posture and chest expansion. Good posture is important because it can help prevent abnormal bending of the spine . Maintaining chest expansion will help prevent problems such as lung infection (pneumonia). It’s a good idea to lie on your stomach a few times each day to keep your spine and hips extended.
- For sleeping, choose a firm mattress and a small pillow that supports your neck.
- Using assistive devices such as canes or walkers. Your local chapter of the Arthritis Foundation, your physical therapist, or a medical supply company may be able to help you find assistive devices in your area.
- If your neck is becoming stiff, your doctor may recommend that you wear a soft neck brace when you ride in the car, to prevent injury in case of an accident .
- Avoid smoking
- See your ophthalmologist for regular eye exams.
- Joining a support group.
MEDICAL TREATMENT:
- Non-steroidal anti-inflammatory drugs (NSAIDs)
- Corticosteroids.
- Muscle relaxants.
- Opioids.
PHYSIOTHERAPY TREATMENTS:
- Regular physiotherapy is very essential in the management of a patient of AS and only physiotherapist is the person who can help the patient to fight with the disease.
Aims of physiotherapy management in ankylosing spondylitis treatment:-
- Relieve pain.
- Maintain the mobility of joints affected like spine, hip, thorax, shoulder etc.
- Prevent and correct deformity.
- Increase chest expansion and vital capacity.
- Attention to posture.
- To maintain and improve physical endurance.
- Advice to patient.
General instruction to patients:
- Make the exercise part of your daily routine.
- Try to do a complete set of exercises at least twice daily at a time convenient to you.
- Heat and cold application any precede exercises to enhance relaxation and decrease pain.
- Perform only those exercises given to you by your physiotherapist.
- Perform exercises on a firm surface.
- Exercise slowly with a smooth motion, do not rush.
- Avoid holding your breath while exercising.
- Modify the exercise regime during an acute attack and contact your physical therapist if you have any complaints or problems with the exercises.
Pain Relief:
Pain and muscle spasm are treated by the following modalities and the relaxation is advised-
- Infra red.
- Hot packs.
- Cryotherapy.
- Steam bath.
- Hydrotherapy.
Exercises for mobilization of joints:
- Maintaining the mobility of joints, by giving mobility exercises to particular joints, which are affected like, spine, hip, shoulder, thoracic cage are essential in Ankylosing Spondylitis Treatment.
- Maintenance of the mobility is very important and the basic aim is that all the joints are moved to their maximum limit and by this, we can delay the process of ankylosis.
Prevent and correct deformity by giving attention to posture:
- The spondylitic patient should always be conscious of his posture while sitting, standing and walking patient should maintain the erect posture during these activities. This helps to prevent and correct deformity and thus help in Ankylosing Spondylitis Treatment.
- Sleeping should occur in prone position or supine on a firm mattress with a thin or no pillow by this, the spine remain in extended position and not in flexion.
- The design of chairs is important particularly for those who spend most of their working hours sitting at desk. Low arm chair should be avoided, an upright chair with some cushioning to support the lower lumber spine is better.
- Adjust the height of the working table and ensure that the patient does not stoop on that.
- Avoidance of prolonged immobilization or bed rest, because of this, the spinal extensors become weak and by this the extended position of the spine is not retained.
Increase chest expansion and vital capacity:
To increase the chest expansion and vital capacity, the breathing exercises are required. Breathing exercises that are used in Ankylosing Spondylitis Treatment:
- Apical breathing exercises.
- Diaphragmatic breathing exercises.
- Lateral costal breathing exercises.
- Deep breathing exercises are encouraged. Ballooning exercise is also very useful in Ankylosing Spondylitis Treatment. They increase the vital capacity of the lung. Thoracic mobility exercises.
Group Therapy Classes:
- The patient can give support to the other member of the class that is another patient.
- Shared problems providing a good medium for patient’s education and latest information about the disease process.
- Development of competitiveness and motivational aspects.
- Improvement in physical fitness.
Exercises :
Forward and Backward Tilt
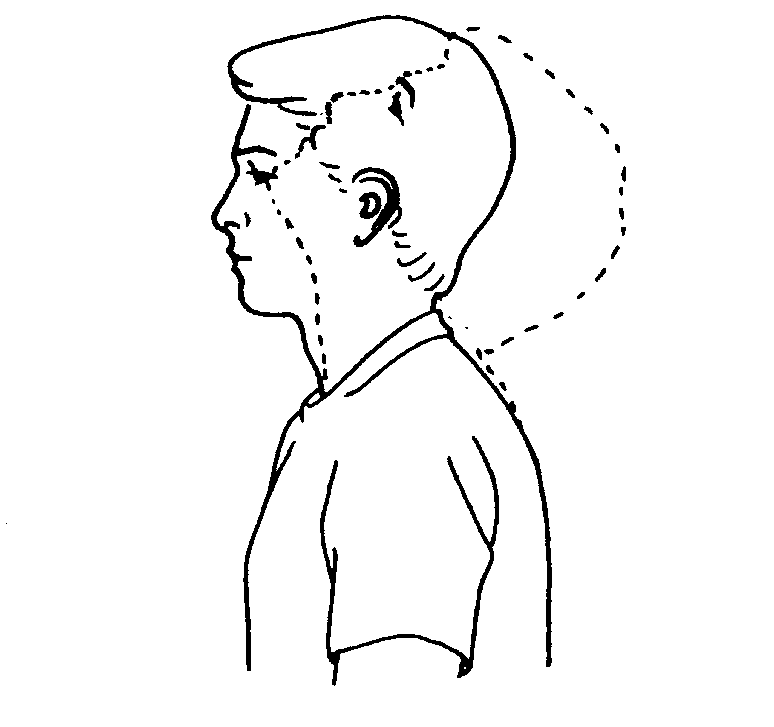
This can be done while you’re seated or on your feet. Keep your moves slow and smooth.
Start with your head squarely over your shoulders and your back straight.
Lower your chin toward your chest and hold for 15-30 seconds. Relax, and slowly lift your head back up.
Tilt your chin up toward the ceiling and bring the base of your skull toward your back. Hold for 10 seconds, then return to the start position.
Repeat the set several times. Do it every day.
Side Tilt
Do this while standing, with your feet hip-width apart and arms down by your sides.
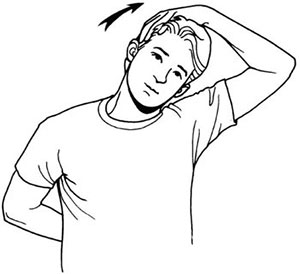
Gently tilt your head toward your right shoulder and try to touch it with your ear. Stop when you feel the stretch. Don’t raise your shoulder.
Hold the stretch for 5-10 seconds, then return to the start position.
Repeat on your left side. You can do several sets and work your way up to 10 repetitions.
For extra stretch, put the hand on the same side of your tilted head on top of your head, and press lightly with your fingertips.
Above Head Stretch :
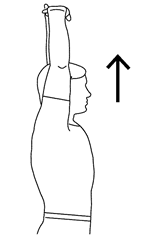
Seated or standing, interlock your fingers, bend your elbows and raise your arms above your head.
Gently squeeze your shoulder blades together and move your elbows and hands backward.
Vary the height of your hands to emphasize shoulders and/or chest (hands behind head, hands on top of head, hand a few inches above head).
Anterior deltoid stretch

You can perform the anterior deltoid stretch standing or seated — just keep your feet firmly planted and your back straight.
With your spine straight, reach your arms behind you and interlace your fingers. If you can’t interlace your fingers, grab opposite wrists or elbows or try grasping a small towel with each hand.
Roll your shoulders back to sit up tall, allowing your chest to open up, and gently squeeze your shoulder blades together.
Moving slowly, carefully straighten your arms.
Next, gradually begin to raise your arms behind you, moving only as far as you can maintain an upright posture. Stop once you feel a stretch.
Pause, breathing deeply into the stretch.
Repeat 2 to 3 times, as needed.
Posterior deltoid stretch
To perform the posterior deltoid stretch, start in a standing or seated position with your spine straight.
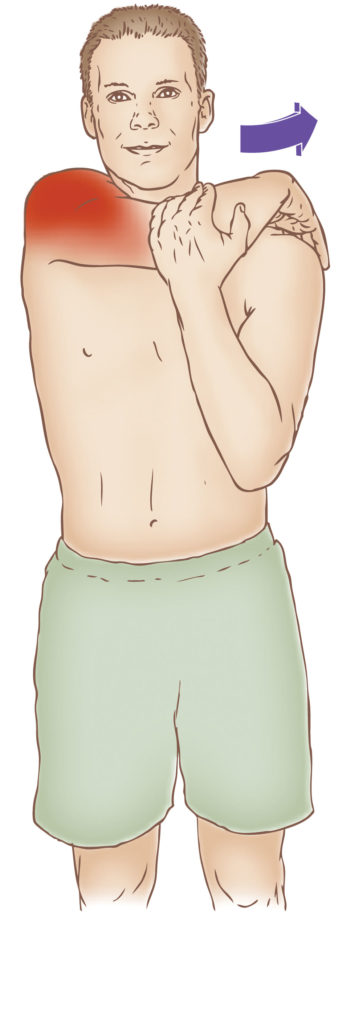
Relax your shoulders.
Reach one arm across your body, using your other arm or wrist to hold it gently by your upper arm.
Slowly begin to pull your arm toward your chest, as far as possible, allowing the stretch to reach deep into the back of your shoulder.
Pause, breathing deeply into the stretch. Hold for at least 30 seconds.
Release and repeat with the other arm.
Overhead triceps stretch
You can do the overhead triceps stretch while standing or sitting.
To do this:

Lift your shoulders up toward your ears and then draw them down and back.
Extend your right arm to the ceiling, then bend at the elbow to bring the right palm toward the center of your back, resting your middle finger along your spine.
Use your left hand to gently push your elbow in toward the center and down.
Hold this stretch 30 seconds for three to four repetitions on each side.
Seated Lateral Trunk Stretch
While in a seated position, raise one arm over your head.
Place your other hand on your thigh for support.
Slowly bend to the opposite side until you feel a comfortable stretch along the side of your trunk.
Hold the stretch for 15-20 seconds, then repeat 3-5 times on each side.
Prayer Stretch
Tucking legs underneath, sit back on the heels and bend forward at the waist, extending arms out over the head onto the floor in front. (The goal is to get length in the lower back muscle). Hold for 30-60 seconds and sit back up. Repeat 3-5 times.

Aerobics Exercise :
Marching in Place :
Stand, holding onto a supportive railing or the back of a chair or bench.
Hold on with both hands if you feel unsteady.
Alternate lifting knees up and down as if marching in place.
March in place for 3 to 5 minutes.
Gradually try to lift knees higher and/or march faster toward the end.
Tap up and tap down :
Stand in front of a box or other stable platform.
Place one foot on the top of the platform. The ball of your foot will be touching the box or ball. Your other foot will remain planted on the ground, and arms at your sides.
To start the exercise, push off from the planted foot to bring it up and onto the platform while simultaneously bringing the lead foot back to the floor. This change will happen mid-air.
Land with the lead foot on the ground and the edge of the planted foot on the platform.
Continue alternating feet, without stopping, for the desired time. The change will be quick, and it will feel like running on stairs. Perform standing toe taps for 30 to 60 seconds. Rest for 15 to 30 seconds and repeat for 2 to 3 sets.
To make this move more challenging, increase the speed of the toe taps and pump your arms.
To decrease some of the difficulty, you can also perform toe taps on the ground doing the same movements without a raised step.
Basic :
It can be done with the R or L foot leading. Step up with one foot and then down (different instructors may use different arm movements with this move).
Example: Basic Right – step up with the R foot first followed by the L foot. Step down with the R foot first followed by the L foot.
V-Step :
The V-Step forms the letter V with the feet and can be done on the aerobic bench or on the floor. You do the movement in four counts.
HOW TO DO IT: Stand with your feet hip-distance apart. Step forward with the right foot as wide as possible, then step forward and out with the left foot as wide as possible. Step right foot and left foot back to hip-distance, one count at a time. Repeat for the designated number of reps.
Turn-step
Do the turnstep on an aerobic bench, also in four counts. Start the move facing the step sideways.
HOW TO DO IT: Leading with the right foot, step up on right corner of the bench sideways. Then bring the left foot up onto the bench to the left corner as you turn. Step off the bench with the right foot, bring the left foot down next to the right foot. Repeat with the left side for as many repetations as desired.
Grapevine
The Grapevine is a popular move in floor-based aerobics classes. It’s performed in an eight-count pattern as you basically criss-cross step across the floor.

HOW TO DO IT: Start with your feet hip-distance apart. Step to the side with the right foot. Step the left foot behind and past the right foot, then step to the side with the right foot. Finally, bring the left foot next to the right foot. Then step to the side with the left foot, bring the right foot behind and past the left foot. Repeat, leading with the left foot and traveling to the left. You may see instructors add turns and bringing the knees up to make the move more challenging.

0Comments