Myelopathy is a term used to describe any neurologic deficit related to the spinal cord. It is usually due to compression of the spinal cord by osteophyte or extruded disc material. It is most commonly localised in the cervical spine but it can also occur in the thoracic and lumbar spine.[1]
There are many primary infectious, inflammatory, neurodegenerative, neoplastic vascular, idiopathic and nutritional disorders that result in myelopathy. These causes are much less common than discogenic diseases, metastases, or trauma. Further explanations will be given in the following paragraphs.
To determine the grade of severity of the myelopathy you can use the Nurick classification. The classification is based on abnormalities in the patient’s gait.[2] This evaluation has demonstrated its sensitivity and validity.
The diagnosis of myelopathy depends on the neurological localization in the spinal cord, rather than the brain or peripheral nervous system. Also, the presence or absence of significant pain or trauma and the mode of onset is primordial to assess the myelopathy into clinical categories.
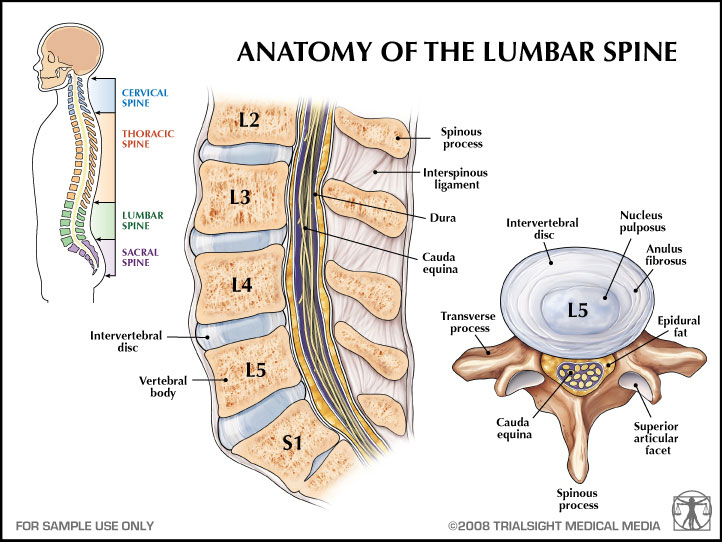
Clinically Relevant Anatomy
The spinal column begins in the cervical region under the skull. It continues into the thoracic region and finally into the lower back where it connects to the sacrum and pelvis. The cervical region consists of 7 vertebrae, the thoracic region of 12 vertebrae and the lumbar region of 5 vertebrae.
Between the corpus and the process of the vertebrae is the spinal canal. It’s a region in the middle of the spine where the spinal cord goes down and nerves travel toward the extremities. The brain and the spinal cord are packed in 3 membranes: dura mater, arachnoid mater and pia mater. Each one has their own structure and function.
Even though the spinal cord is well protected, it can be damaged by epidural or intradural causes. This is what’s happens when we’re talking about myelopathy.
Epidemiology /Etiology
Myelopathy can sometimes be a slow process. The symptoms can develop slowly over a period of months or it can go very fast.
It’s difficult to clinically distinguish myelopathy from other non-traumatic causes of myelopathy because the classic history is frequently absent or difficult to elicit from a seriously ill patient.
There are many risk factors that may cause or occur thoracic myelopathy.
Thoracic myelopathy occurs because of:
• Discus hernia
• Spinal degeneration
• Facet degeneration
• Ligamentum flavum hypertrophy
• Calcification of ligamentum flavum
• Compression due to extradural mass (Spinal tumours)
• Posttraumatic deformities
• Infections
• Angular kyphosis (congenital, tuberculous, neurofibromatosis and posttraumatic kyphosis)
• Vascular disorders (vascular malformations, spinal cord infarct and epidural hematoma)
• Nutritional disorders
Risk factors:
1. Age
2. Degrees of motor and sensory deficits
Degrees of spinal cord compression, absence of proximal stenosis and intramedullary hypertension this factors predicted the surgical outcome.
Characteristics/Clinical Presentation
Following characteristics may occur
• Muscle weakness
• Altered muscle tonus
• Sensory loss (in trunk and legs) and spasticity
• Impaired coordination
• Walking problems
• Backache
• Urinary disturbances
Cook et al. describe the following Cluster to Identify the presence of Cervical Myelopathy:
- Hoffmann's Sign Test
- Cervical Deep Tendon Reflex Test
- Inverted Supinator Test
- Suprapatellar Quadriceps Test
- Hand Withdrawal Reflex Test
- Babinski Sign Test
- Clonus of the Ankle Test
- Any 1 of 2 positive Inverted Supinator (IVS) and Suprapatellar reflex
- 2 of 2 positive Babinski sign and (IVS):
- 2 of 3 positive Babinski sign, Hoffmann's Relfex and (IVS):
- 3 of 4 Hoffmann's Relfex, Suprapatellar reflex, Babinski, and (IVS):
Differential Diagnosis
It can be difficult to diagnose myelopathy because the clinical presentations are variable and sometimes like those of other disorders. That’s why it’s important to have a thorough history and complete physical examination of the patient. In this case, it is very difficult to know which symptoms appear by myelopathy or to the mediated disorders.
Other pathologies that can be involved in myelopathy are:
• Spinal stenosis
• Discus hernia
• Spondylolistheses
• Discus bulging
Diagnostic Procedures
Diagnosis of myelopathy depends on the neurologic localization. Imaging of the myelopathy is crucial.
Primary method:
Magnetic resonance imaging (MRI)
This can show a reduced spinal cord diameter or abnormalities in the cord and hypertension in the central cord.
Other methods:
1. Computed tomography (CT) - You can see bony injuries or ligamentous injuries when they are present
2. Myelogram
3. Radiographs - Radiography may depict osteophytic narrowing of the spinal canal or bone destruction
Outcome Measures
- Nurick classification
- The Japanese Orthopedic Association scale (JOA)
- ODI
- VAS – scale
Examination
Diagnosis of myelopathy rest on demonstration of mechanical stability of the spine. We should note that MRI is considered as the golden standard to diagnose myelopathy. Physical examination results commonly in long tract signs such as spasticity, hyperreflexia and abnormal reflexes. Hoffmann, Babinski, and clonus are frequently tested reflexes. Someone with myelopathy has a positive Hoffman and/or Babinski and/or clonus test. We also frequently notice progressive deterioration in their hand and gait function. So, it can be useful to examine the gait cycle of the patient with a toe-to-heel walk and the Romberg test.
Myelopathy leads to generalized weakness and intrinsic muscle wasting. That’s why it’s also important to test some muscles with tests such as the Finger escape sign or the Rapid grip and release test.
The Japanese Orthopaedic Association scale can help us to assess the severity of clinical symptoms in patients with myelopathy. It consists of 6 scales (motor dysfunction in upper extremities, motor dysfunction in the lower extremities, sensory function in the upper extremities, sensory function in the trunk, sensory function in the lower extremities and bladder function) based on motor and sensory functions which are individually graded with a maximal score of 17. We should note that there exists a modified Japanese Orthopaedic Association score used in Europe. The two scores showed a good correlation with each other in terms of their total scores and recovery rates.
More specific information about physical examination for cervical myelopathy can be read on this page.
Medical Management
Conservative management, such as physical therapy, cervical immobilisation or anti-inflammatory medication is preferred. But when patients have intractable pain or progressive neurological symptoms surgical interventions are needed. As we mentioned above myelopathy is usually due to compression. When surgical intervention is needed, we will focus on decompression of the spinal cord and nerve roots. Deformity prevention by maintaining or supplementing spinal stability will be another goal of this intervention. There are many techniques describes decompressing the spinal cord and roots which can be anterior, posterior focus circumferential. The choice of the most effective technique is dependent on numerous factors such as location, comborbidity, stability of spinal column and surgeon’s experience.
The following surgical techniques can be used to decompress the spinal cord:
- Laminectomy, a posterior approach thas has been proven to be a safe and effective technique
- Laminoplasty, a posterior approach developed to allow cord decompression while preserving motion with less substantial alteration of the natural biomechanics
- Anterior Cervical Discectomy, effective for ventral pathology such as osteophyte or disc complexes
Anterior Cervical Corpectomy, effective in pathology extends beyond the spine interspaces
When we look at the efficacy of a laminectomy and a laminoplasty we see that they both show an improvement in clinical disease severity, functional status and quality of life as far as 24 months of measurements show in patients with degenerative cervical myelopathy.
When we look at to the differences between anterior and posterior laminectomy in patients with cervical spondylotic myelopathy, we see that there are none concerning the health-related outcome measurements. We do see that the anterior approach is more often used in younger patient weer the myelopathy is less severe.
When we look at compressive myelopathy, at first we see that lumbar spine stenosis can be a risk factor. Secondly, we see that metastatic compression of the spinal cord can occur in myelopathy.
Lumbar spinal stenosis can be treated conservatively with the use of medications which will focus on increasing the blood vessel diameter and with this the blood flow. This because the diameter of the blood vessels in the cauda equina in LSS patiënts is significantly smaller than the diameter of blood vessels in healthy individuals.
- Medication : vitamins, NSAID’s, muscle relaxants and prostaglandines.
Non-operative treatment also consists of physical therapy, epidural injection and facet joint injections. When doing a follow up (until 6 months) on LSS patients who underwent non-surgical treatment, we conclude that there is a significant pain relief and improvement in physical function 3 months follow up and a significant improvement in COMI scores on a 6-month follow-up.
There is no difference found between treating LSS patients with epidural steroid injections and physical therapy, both of whom are supplemented with a home-based exercise program and received diclofenac. Although both treatments didn’t differ, they showed a significant improvement with the controle group.
Lumbar spinal stenosis can be treated surgically by the decompressive mild procedure. This is a minimally invasive procedure in which they will remove part of the posterior fibers of the hypertrophic ligamentum flavum and some interlaminar bone while maintaining anatomy, stability and biomechanics of the lumbar spine.
The use of the decompressive mild procedure is shown that in comparison with an open laminectomy surgery laminectomy :
- There are fewer complications
- There are less / none instability problems found post-operative
- have a shorter operating length
- have less blood loss
- hospitalisation time is smaller (the same day released)
- patient safety is much better
When the mild procedure is used, there is a continuous epidurographic lateral oblique fluoroscopic imaging.
Metastatic spinal cord compression is another cause for compressive myelopathy. Spinal tumours are classified in 3 sorts: extradural, intradural extramedullary an intradural intramedullary. This Metastatic spinal cord compression is diagnosed in 2,5 –5% of the cancer patients. The type of medical management of these tumours will depend on the stability of the spine, neurological and pain status. Surgical intervention is indicated when :
- patient experiences paraplegia not more than 12 – 24 hours
- spinal instability
- bony compression of the spinal cord
A surgical intervention is performed to preserve neurological function and pain and will improve median survival rates for at least 6 months. Post-operative complications are respiratory complications, deep venous thrombosis, pulmonary embolism, cerebrospinal fluid leak and wound infection.
Radiation therapy can be applied post-operatively and can have beneficial effects when used in combination with corticosteroids or with Dexamethasone is used before radiotherapy (higher ambulatory rate).
In a patient with a good prognosis, radiotherapy is indicated to relief pain, preserve or improve neurological function. In patients with poor prognosis, who have a life expectancy of 6 months, radiotherapy will not help on the matter of neurological function and will just offer pain relief. Single-dose radiation is associated with higher in-field recurrence.[1]level of evidence 1A
Physical Therapy Management
As we know many causes can result in myelopathy. This is why it’s difficult to treat myelopathy. Before we treat the myelopathy we have to have an idea about the aetiology. It has also been reported that symptoms of mild myelopathy have been improved by conservative treatment in a high ratio of patients. Also, continuous traction of the spine improves myelopathy symptoms.
Spondylotic myelopathy
On the information based on a case report, physical therapy can achieve satisfactory results in patients with spondylotic myelopathy. Unfortunately, the complete reduction in symptoms was not achieved. It’s reported that in the initial phase manual therapy techniques can be employed to reduced pain. The goal of the therapy is to give some space. So extension and rotation at the painful level can be useful.[20] Hypothesis has been raised to explain the reduced pain and the improved function achieved with manual therapy.[21]
In the second phase, manual therapy can be necessary but is not the main part of the therapy. This phase consisted of dynamic upper and lower limb exercises and functional or primitive diagonals of PNF for the upper and lower limbs.
In a final phase, the therapist can involve aerobic exercise like 20min on a treadmill, balance training like standing on one leg with eyes open or closed and core stability exercises like the back bridge or side bridge.
Another study reported that we have to note that the number of patients undergoing conservative treatment for spondylotic myelopathy is decreasing because of the improvement in recent surgical results. This study performed continuous traction by the Good-Samaritan method of the spine if patient desired it. It was performed for 3-4 hours daily. This was in combination with drug therapy and exercise therapy. Conservative treatment for CSM is considered to be effective if it is performed intensively selected patients.
Surgery is indicated when the symptoms are not improved or are exacerbated. So only patients who responded well to conservative treatment are followed up for a long period.
Viral myelopathy
As far as we are only a few studies have considered the results of physiotherapy on viral myelopathy specifically patients with T-lymphotropic virus 1. Physical exercises have shown the best results. Therefore only a simple protocol of six functional exercises look to have a positive impact on functionality. This protocol included using stairs, standing on tiptoes, squatting, sitting and standing.
Degenerative myelopathy
When we look at the effects of physical therapy pre –and post-surgical to patients with degenerative lumbar disorders, we see that there is little evidence to describe the physical therapy that is used. Some researchers suggest that when early rehabilitation and early exercise are given post-operative, the patient will resume work activity, are discharged earlier from hospitalization and reach some of the measured post-operative milestones earlier

0Comments