Respiratory failure is classified according to blood gases abnormalities into type 1 and type 2.Respiratory failure is a clinical condition that happens when the respiratory system fails to maintain its main function, which is gas exchange, in which PaO2 is lower than 60 mmHg and/or PaCO2 higher than 50 mmHg.
 |
| Respiratory failure |
Type 1: (hypoxemic) respiratory failure has a PaO2 < 60 mmHg with normal or subnormal PaCO2. In this type, the gas exchange is impaired at the level of aveolo-capillary membrane. Examples of type I respiratory failures are carcinogenic or non-cardiogenic pulmonary edemaa, ARDs, COVID-19 and severe pneumonia.
Type 2: (hypercapnic) respiratory failure has a PaCO2 > 50 mmHg. Hypoxemia is common, and it is due to respiratory pump failure.
- RF a major cause of mortality and morbidity and mortality rates increase with age and presence of co-morbidities.
Pathophysiology
The main pathophysiologic mechanisms of respiratory failure are:
- Hypoventilation: in which PaCO2 and PaO2 and alveolar-arterial PO2 gradient (difference between the calculated oxygen pressure available in the alveolus and the arterial oxygen tension, measures the efficiency of gas exchange). are normal. Depression of CNS from drugs (eg opiod use disorder) is an example of this condition.
- V/P mismatch: this is the most common cause of hypoxemia. Administration of 100% O2 eliminates hypoxemia.
- In respiratory physiology, the ventilation/perfusion ratio (V̇/Q̇ ratio or V/Q ratio) is a ratio used to assess the efficiency and adequacy of the matching of two variables:V (ventilation) the air that reaches the alveoli; Q (perfusion) the blood that reaches the alveoli via the capillaries. V/Q ratio is defined as the ratio of the amount of air reaching the alveoli per minute to the amount of blood reaching the alveoli per minute. These two variables, V & Q, constitute the main determinants of the blood oxygen (O2) and carbon dioxide (CO2) concentration.
- Shunt (pathological condition in which the alveoli are perfused but not ventilated) : in which there is persistent hypoxemia despite 100% O2 inhalation. In cases of a shunt, the deoxygenated blood (mixed venous blood) bypasses the alveoli without being oxygenated and mixes with oxygenated blood that has flowed through the ventilated alveoli, and this leads to hypoxemia as in cases of pulmonary edema (cardiogenic or noncardiogenic), pneumonia and atelectasis
Types
- Type I respiratory failure involves low oxygen, and normal or low carbon dioxide levels. Occurs because of damage to lung tissue eg including pulmonary oedema, pneumonia, acute respiratory distress syndrome, and chronic pulmonary fibrosing alveoloitis. This lung damage prevents adequate oxygenation of the blood (hypoxaemia); however, the remaining normal lung is still sufficient to excrete the carbon dioxide being produced by tissue metabolism. This is possible because less functioning lung tissue is required for carbon dioxide excretion than is needed for oxygenation of the blood.
- Type II respiratory failure involves low oxygen, with high carbon dioxide (pump failure). It occurs when alveolar ventilation is insufficient to excrete the carbon dioxide being produced. The most common cause is chronic obstructive pulmonary disease (COPD). Others include chest-wall deformities, respiratory muscle weakness (e.g. Guillain-Barre syndrome) and central depression of the respiratory centre (e.g. heroin overdose) Inadequate ventilation is due to reduced ventilatory effort, or inability to overcome increased resistance to ventilation – it affects the lung as a whole, and thus carbon dioxide accumulates. Complications include: damage to vital organs due to hypoxaemia, CNS depression due to increased carbon dioxide levels, respiratory acidosis (carbon dioxide retention). This is ultimately fatal unless treated. Complications due to treatment may also occur.
Epidemiology
Overall frequency of respiratory failure is not well known as respiratory failure is a syndrome not a single disease process[2].
Etiology
 |
| Respiratory Failure |
Respiratory failure may be due to pulmonary or extra-pulmonary causes which include:
- CNS causes due to depression of the neural drive to breath as in cases of overdose of a narcotic and sedative.
- Disorders of the peripheral nervous system: Respiratory muscle and chest wall weakness as in cases of Guillian-Barre syndrome and myasthenia gravis.
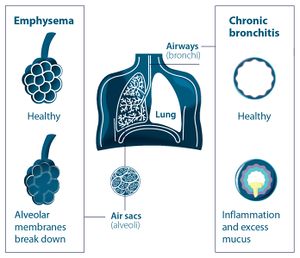
- Upper and lower airways obstruction: due to various causes as in cases of exacerbation of chronic obstructive pulmonary diseases and acute severe bronchial asthma
- Abnormities of the alveoli that result in type 1 (hypoxemic) respiratory failure as in cases of pulmonary edema and severe pneumonia
Clinical Presentation
Presentation of respiratory failure is dependent on the underlying cause and associated hypoxemia or hypercapnia.
Common presentations include:
- Dyspnoea
- Tachypnoea
- Restlessness
- Confusion
- Anxiety
- Cyanosis- central
- Tachycardia
- Pulmonary hypertension
- Loss of consciousness
Signs and symptoms of RF Type I (Hypoxemia) include:
- Dyspnea, irritability
- Confusion, fits, somnolence
- Tachycardia, arrhythmia
- Tachypnea
- Cyanosis
Signs and symptoms of RF Type II (Hypercapnia) include[4]:
- Change of behavior
- headache
- Coma
- Warm extremities
- Astrexis
- Papilloedema
Symptoms and signs of the underlying disease:eg
- Fever, cough, sputum production, chest pain in cases of pneumonia.
- History of sepsis, polytrauma, burn, or blood transfusions before the onset of acute respiratory failure may point to acute respiratory distress syndrome
Physical Findings
These are signs that suggest a possible underlying cause of respiratory failure include:
- Hypotension usually with signs of poor perfusion suggest severe sepsis or pulmonary embolus
- Hypertension usually with signs of poor perfusion suggests cardiogenic pulmonary edema
- Wheeze & stridor suggest airway obstruction
- Tachycardia and arrhythmias may be the cause of cardiogenic pulmonary edema
- Elevated jugular venous pressure suggests right ventricular dysfunction
- Respiratory rate < 12b/m in spontaneously breathing patient with hypoxia or hypercarbia and acidemia suggest nervous system dysfunction
- Paradoxical respiratory motion suggest muscular dysfunction
- see also A-E respiratory assessment
Evaluation
Respiratory Failure
Arterial blood gases- measures oxygen and carbon dioxide levels in the blood- Renal function tests and liver function tests- may indicate the etiology of respiratory failure or identify complications associated with it.
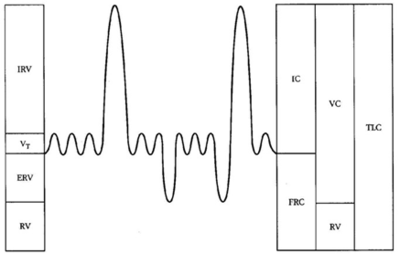
- Pulmonary Function Test- identifies obstruction, restriction, and gas diffusion abnormalities. Normal values for forced expiratory volume in 1 second(FEV1) and forced vital capacity(FVC) suggest a disturbance in respiratory control. Decrease in FEV1 to FVC ratio indicates airflow obstruction. A decrease in FEV1 and FVC and maintenance of FEV1 to FVC ratio suggest restrictive lung disease.
- Electrocardiography(ECG)
- Chest radiography is needed as it can detect chest wall, pleural and lung parenchymal Lesions.
Other investigations needed for detecting the underlying cause of the respiratory failure may include:
- Complete blood count (CBC)
- Sputum, blood and urine culture
- Blood electrolytes and thyroid function tests
- Echocardiography
- Bronchoscopy
Complications
Multiple organ-system complications involving the cardiovascular, pulmonary, gastrointestinal system may occur subsequent to respiratory failure
- Pulmonary: pulmonary embolism, pulmonary fibrosis, complications secondary to the use of mechanical ventilator
- Cardiovascular: hypotension, reduced cardiac output, cor pulmonale, arrhythmias, pericarditis and acute myocardial infarction
- Gastrointestinal: haemorrhage, gastric distention, ileus, diarrhoea, pneumoperitoneum and duodenal ulceration- caused by stress is common in patients with acute respiratory failure
- Infectious: noscomial- pneumonia, urinary tract infection and catheter-related sepsis. Usually occurs with use of mechanical devices.
- Renal: acute renal failure, abnormalities of electrolytes and acid-base balance.
- Nutritional: malnutrition and complications relating to parenteral or enteral nutrition and complications associated with NG tube- abdominal distention and diarrhea
Management
This includes supportive measures and treatment of the underlying cause.
Supportive measures which depend on depending on airways management to maintain adequate ventilation and correction of the blood gases abnormalities
Correction of Hypoxemia
Respiratory Failure
- The goal is to maintain adequate tissue oxygenation, generally achieved with an arterial oxygen tension (PaO2) of 60 mm Hg or arterial oxygen saturation (SaO2), about 90%.
- Un-controlled oxygen supplementation can result in oxygen toxicity and CO2 (carbon dioxide) narcosis. Inspired oxygen concentration should be adjusted at the lowest level, which is sufficient for tissue oxygenation.
- Oxygen can be delivered by several routes depending on the clinical situations in which we may use a nasal cannula, simple face mask nonrebreathing mask, or high flow nasal cannula.
- Extracorporeal membrane oxygenation may be needed in refractory cases
2. Correction of hypercapnia and respiratory acidosis
- This may be achieved by treating the underlying cause or providing ventilatory support.
3. Ventilatory support for the patient with respiratory failure
The goals of ventilatory support in respiratory failure are:
- Correct hypoxemia
- Correct acute respiratory acidosis
- Resting of ventilatory muscles[
Non-invasive respiratory support: is ventilatory support without tracheal intubation/ via upper airway. Considered in patients with mild to moderate respiratory failure. Patients should be conscious, have an intact airway and airway protective reflexes. Noninvasive positive pressure ventilation(NIPPV) has been shown to reduce complications, duration of ICU stay and mortality(). It has been suggested that NIPPV is more effective in preventing endotracheal intubation in acute respiratory failure due to COPD than other causes. The etiology of respiratory failure is an important predictor of NIPPV failure.
Invasive respiratory support: indicated in persistent hypoxemia despite receiving maximum oxygen therapy, hypercapnia with impairment of conscious level. Intubation is associated with complications such as aspiration of gastric content, trauma to the teeth, barotraumas, trauma to the trachea etc
- Permissive hypercapnia - A ventilatory strategy that allows arterial carbon dioxide(PaCO2) to rise by accepting a lower alveolar minute ventilation to avoid the risk of ventilator-associated lung injury in patients with ALI and minimize intrinsic positive end-expiratory pressure (auto PEEP) in patients with COPD thereby protecting the lungs from barotrauma. Permissive hypercapnia could increase survival in immunocompromised children with severe ARDS
Physiotherapy Management
Physio-therapeutic interventions aim to maximize function in pump and ventilatory systems and improve quality of life.
- In mechanically ventilated patients, early physiotherapy has been shown to improve quality of life and to prevent ICU-associated complications like de-conditioning, ventilator dependency and respiratory conditions.
- Main indications for physiotherapy are excessive pulmonary secretions and atelectasis.
- Timely physical therapy interventions may improve gas exchange and reverse pathological progression thereby avoiding ventilation.
Interventions include:
Positioning: the use of specific body position aimed at improving ventilation/perfusion(V/Q) matching, promoting mucociliary clearance, improving aeration via increased lung volumes and reducing the work of breathing. These include:
Respiratory Failure - Prone: helps to improve V/Q matching, redistribute edema and increase functional residual capacity(FRC) in patients with acute respiratory distress syndrome. It has been shown to result in oxygenation for 52-92% of patients with severe acute respiratory failure.
- Side-lying: with affected lungs uppermost to improve aeration through increased lung volumes in patients with unilateral lung disease.
- Semi-recumbent: 450 head-up position serves to prevent the risk of gastroesophageal reflux and aspiration.
- Upright: helps to improve lung volumes and decrease work of breathing in patients that are being weaned from mechanical ventilator.
- Postural drainage and Percussion: uses gravitational effects to facilitate mucociliary clearance
- Suction: used for clearing secretions when the patient cannot do so independently (Guglielminotti et al recommended a saw-tooth pattern seen on ventilator’s flow-volume loop and/or respiratory sounds over the trachea as good indicators for tracheal suction in a ventilated patient).
Manual Hyperinflation: aims to re-inflate atelectatic areas of the lung as such improving pulmonary compliance and facilitate the clearance of pulmonary secretions when used with other techniques.
Respiratory Failure - Active cycle of breathing technique and manual techniques such as shaking and vibration to facilitate mucus clearance
- Limb exercises: passive, active-assisted, active exercises may optimize oxygen transport and reduce the effects of immobility.
- Inspiratory muscle training: aims to improve inspiratory muscle strength and it facilitates weaning from mechanical ventilation. It has be shown to improve whole body exercise performance, particularly in less fit subjects. The study by Hoffman L et showed positive outcomes with inspiratory muscle training in patients with advanced lung disease.
- Early mobilisation: improves function, mobility and quality of life
Differential Diagnosis
- Acute Respiratory Distress Syndrome
- Angina Pectoris
- Aspiration Pneumonitis
- Asthma
- Atelectasis
- Cardiogenic shock
- Obstructive sleep apnea
- Myocardial infarction
- Pulmonary embolism
Prognosis
Respiratory failure is associated with poor prognosis but advances in mechanical ventilation and airway management have improved prognosis. It is dependent on the underlying cause of respiratory failure.
- Mortality rates of approximately 40-45% which has remained constant over the years occur with acute respiratory distress syndrome(ARDS) with younger patients(< 60 years) having better survival rates.
- About two-thirds of the patients who survive an episode of ARDS show some impairment of pulmonary function one or more years of post-recovery.
- For COPD and acute respiratory failure. overall mortality has reportedly declined from 26% to 10%.
- Significant mortality occurs in patients with hypercapnic respiratory failure due to associated co-morbidities and poor nutritional status.


0 Comments