Heart transplantation is the replacement of a failing heart with a heart from a suitable donor. After a decline between 1993 and 2004, heart transplant volumes reported to the International Society of Heart and Lung Transplantion (ISHLT) Transplant Registry have been steadily increasing, especially in recent years, and reached an all-time high in 2016 at a total of 5832 heart transplants from 346 centers.
 |
| Heart Transplant |
Heart transplantation (HTx) has become the preferred therapy for select patients, with a 1-year survival of almost 90% and a conditional half-life (the time at which 50% of patients who survived the first year are still alive) of 13 years. See the image below.
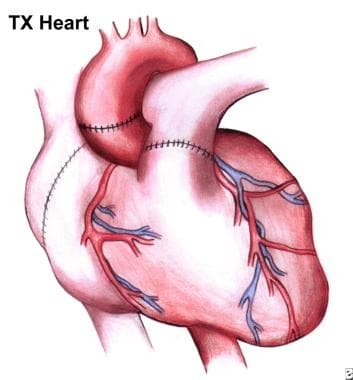 |
| Completed operation. Note suture lines on now-implanted heart. |
Indications for heart transplantation
Heart transplantation is generally reserved for patients with end-stage congestive heart failure (CHF) who are estimated to have less than 1 year to live without the transplant and who are not candidates for or have not been helped by conventional medical therapy. Because of the poor condition of their heart, most heart transplantation candidates are excluded from other surgical options. Specific indications for a transplant include the following:
Dilated cardiomyopathyIschemic cardiomyopathy
Congenital heart disease for which no conventional therapy exists or for which conventional therapy has failed
Ejection fraction of less than 20%
Intractable angina or malignant cardiac arrhythmias for which conventional therapy has been exhausted
Pulmonary vascular resistance of less than 2 Wood units
Age younger than 65 years
Ability to comply with medical follow-up care
Workup
Evaluation of the heart transplant candidate includes laboratory tests, imaging studies, and other tests as appropriate.
Laboratory studies
Virus: Including hepatitis viruses, human immunodeficiency virus (HIV), Epstein-Barr virus (EBV), and cytomegalovirus (CMV); used to determine past exposure and currently active diseaseFungus and tuberculosis (TB): Used to determine past exposure and to predict reactivation
Prostate-specific antigen (PSA): If elevated, initiate appropriate evaluation and therapy before completing the evaluation for transplantation
Papanicolaou test: Results should be negative before listing for transplantation
Complete blood count (CBC): With differential, platelet count, prothrombin time (PT), activated partial thromboplastin time (aPTT), and a complete chemistry profile (including liver panel, lipid profile, and urinalysis)
Blood typing and screening, panel-reactive antibody (PRA) testing, and tissue typing: Used to determine the immunologic suitability of the patient for transplantation and donor matching
Imaging studies
Coronary arteriography: Performed in cases of cardiomyopathy to determine if the cause of the cardiac dysfunction may be amenable to conventional therapiesEchocardiography: Used to determine the cardiac ejection fraction and to monitor the cardiac function of patients on the transplantation waiting list
Posteroanterior and lateral chest radiographs: Used to screen for other thoracic pathologies that may preclude transplantation.
Bilateral mammograms: Should reveal no abnormalities before listing for transplantation
Cardiac and pulmonary evaluation
Maximal venous oxygen consumption (MVO2): Used to assess overall cardiac function and as a predictor of the severity of congestive heart failure and survivalBiopsy
Endomyocardial biopsy of the potential candidate is not routinely performed. The procedure may be considered if a systemic process involving the heart is thought to be the cause of the cardiomyopathy.
Perform biopsies of appropriate areas if the patient exhibits symptoms of systemic disease. Biopsies are used to determine the extent and activity of the disease process. Systemic disease processes are a contraindication to cardiac transplantation.
 |
| Heart Transplants |
Transplantation procedures
During the cardiac transplantation procedure, the ventricles are excised, leaving the great vessels, right atrium, and left atrium of the recipient. The donor heart is then sewn to these areas. A cardiac allograft can be sewn in either a heterotopic or an orthotopic position.
Heterotopic heart transplantation
Heterotopic transplantation is an excellent technique for patients with severe pulmonary hypertension. Inherent problems with the technique, however, include pulmonary compression of the recipient, difficulty obtaining an endomyocardial biopsy, and the need for anticoagulation.
Orthotopic heart transplantation
Orthotopic heart transplantation is performed with either of the following techniques:
Shumway-Lower technique: This method is simpler and saves perhaps 10-15 minutes of ischemic timeBicaval anastomosis: One advantage of the bicaval method is that, by avoiding a large right atrium, the surgeon can maintain better atrial transport; another claimed advantage of this technique is a lower reported incidence of tricuspid regurgitation
Immunosuppressive therapy
Immunosuppression is started soon after surgery. Several regimens can be used, including pretransplantation induction therapy and simple postoperative maintenance therapy; the choice of regimen depends on the training and experience of the transplant center.
Most maintenance immunosuppressive protocols after HTx use a 3-drug regimen consisting of a calcineurin inhibitor (CNI) (cyclosporine or tacrolimus), an antimetabolite agent (mycophenolate mofetil or azathioprine), and tapering doses of corticosteroids over the first year post-transplantation.
Complications
Posttransplant complications can include the following:
Bleeding from suture linesHyperacute rejection
Infection
Psychiatric disturbances from steroid therapy
Cardiac rejection
Allograft vascular diseaseatient education




0 Comments