Pott’s fracture, also known as Pott’s syndrome I and Dupuytren fracture, is an archaic term loosely applied to a variety of bimalleolar ankle fractures.
The injury is caused by a combined abduction external rotation from an eversion force.
This action strains the sturdy medial (deltoid) ligament of the ankle, often tearing off the medial malleolus due to its strong attachment.
The talus then moves laterally, shearing off the lateral malleolus or, more commonly, breaking the fibula superior to the tibiofibular syndesmosis.
If the tibia is carried anteriorly, the posterior margin of the distal end of the tibia is also sheared off by the talus.
A fractured fibula in addition to detaching the medial malleolus will tear the tibiofibular syndesmosis.
The combined fracture of the medial malleolus, lateral malleolus, and the posterior margin of the distal end of the tibia is known as a “trimalleolar fracture”.
An example of Pott’s fracture would be in a sports tackling injury.
The player receives a blow to the outside of the ankle, causing the ankle to roll inwards (so that the sole of the foot faces laterally).
This damages the ligaments on the inside of the ankle and fractures the fibula at the point of contact (usually just above the tibiofibular syndesmosis).
A better way to visualize this is the two hands of a clock, with one hand facing 12 and the other facing 6.
The vertical line they form represents the fibula of the person’s right leg.
The lateral force approaches from 3 o’clock, sending the lower hand snapping outwards to point at 5 o’clock.
 |
| Pott's Fracture |
Anatomy
The ankle contains three joints. The talocrural joint or ankle joint is a hinge joint formed between the inferior surface of the tibia and the superior surface of the talus.
The medial and lateral malleoli provide additional articulations and stability to the ankle joint.
The inferior tibiofibular joint is formed by the articulation of the distal parts of the fibula and tibia. The inferior tibiofibular joint is supported by the tibiofibular ligaments or syndesmosis.
The subtalar joint between the talus and calcaneus is divided into an anterior and posterior articulation separated by the sinus tarsi.
The lateral ligament consists of three parts :-
the anterior talofibular ligament which passes as a flat band from the tip of the fibula anteriorly to the lateral talar neck :-
the calcaneofibular ligament, which is a cordlike structure directed somewhat posteriorly;
and the posterior talofibular ligament, which runs posteriorly from the fibula to the talus.
Mechanism of Injury / Pathological Process
A Pott’s fracture is a fracture affecting one or both of the malleoli.
During activities such as landing from a jump (volleyball, basketball) or when rolling an ankle, a certain amount of stress is placed on the tibia and fibula and the ankle joint.
When this stress is traumatic, and beyond what the bone can withstand, a break in the medial, lateral, or posterior malleolus may occur.
Also, activities involving a sudden change of direction, such as football and rugby, can cause fractures around the malleoli.
When this happens, this condition is known as a Pott’s fracture.
A Pott’s fracture often occurs in combination with other injuries such as an inversion injury, a dislocation of the ankle, or other fractures of the foot, ankle, or lower leg.
Pott’s fractures can vary in location, severity, and type including displaced fractures, un-displaced fractures, bi-malleolar fractures, or compound fractures.
It is difficult to distinguish clinically between a fracture and a moderate-to-severe ligament sprain. Both co
nditions may result from inversion injuries, with severe pain and varying degrees of swelling and disability.
Symptoms
A Pott’s fracture occurs from a badly sprained ankle.
it is often difficult to distinguish between a Pott’s fracture and an ankle sprain in the early stages. Symptoms consist of:
Instant and severe pain in the ankle.
You will be unable to put weight on your leg.
There will be tenderness at the point of fracture.
You will have considerable swelling and bruising.
Classification
They have been classified in many ways based on mechanism of injury, joint stability number of malleoli involved or the level of the fracture.
Few of the classification are as under:-
1) Henderson’s Classification
This is the simplest classification based on the number of malleoli fractured when seen on skiagram.
Type 1-Unimalleolar,
Type 2-Bimalleolar
Type 3-Trimalleolar.
This does not deal with fracture pattern, mechanism of injury or the ligamentous injuries.
2) Danis Weber’s Classification

This classification is based on the level of the fracture of the fibula.
Type 1-Fracture of fibula below the level of syndesmosis.
Type 2-Fracture of fibula at the level of syndesmosis.
Type 3-Fracture of fibula above the level of syndesmosis
3) Lauge-Hansen’s Classification
This classification is based on radiographic, clinical and experimental observations . It takes the mechanism of injury into consideration i.e. the position of the foot at the time of injury is described first and the direction of the deforming force later. It has the following types:-
a) Supination-Adduction
There is a transverse avulsion fracture of the lateral malleolus below the level of the syndesmosis or tear of lateral collateral ligament. If the force continues there will be a vertical fracture of medial malleolus.
b) Supination-External Rotation
It leads to disruption of anterior tibio-fibular ligament, spiral oblique fracture of distal fibula, disruption of posterior tibiofibular ligament or fracture of posterior malleolus and fracture of medial malleolus or rupture of deltoid ligament.
c) Pronation-Abduction
It causes transverse fracture of the medial malleolus or rupture of the deltoid ligament, rupture of all syndesmotic ligaments or avulsion fracture of their insertions and a short, horizontal fracture of fibula above the level of syndesmosis.
d) Pronation-External Rotation
This causes transverse fracture of medial malleolus or disruption of the deltoid ligament, disruption of the anterior tibiofibular ligament, short oblique fracture of fibula above the level of the joint.
And if the force continues there is rupture of posterior tibio-fibular ligament or avulsion fracture of the postero-lateral part of tibia.
e) Pronation-Dorsiflexion
This injury causes fracture of the medial malleolus, fracture of anterior margin of tibia, supramalleolar fracture of fibula and transverse fracture of posterior tibial surface.
4) AO’S Classification
This classification is a modification of the Danis Weber classification.
Three main types of the fracture have been described depending on the level of the fibular fracture. Each of these types are further divided into 3 subgroups each.
Type A. Fibular fracture below syndesmosis
A1-isolated
A2-with fracture of medial malleolus
A3-with a postero medial fragment
Type B. Fibular fracture at level of syndesmosis
B1-isolated
B2-with medial lesion
B3-with medial lesion and fracture of posterolateral tibia
Type C. Fibular fracture above syndesmosis
C1-diaphyseal fracture fibula-simple
C2-diaphyseal fracture fibula-complex
C3-proximal fracture fibula
Clinical feature
- pain (sudden,onset,sharp,intense pain over lower ankle / leg ) .
- swelling, burcing .
- crepitus .
- improve rom .
- instability stand / weight bearing .
- deformity .
Clinical Examination
The history of mechanism of injury is important and will tell us the likely pattern of injury sustained to the ankle.
Careful physical examination is needed to see the status of the skin, soft tissues, neurovascular deficit, bones and ligaments.
Stress tests like anterior drawer, inversion, eversion, external rotation can also be done under sedation or anaesthesia to find out details of injuries.
Diagnosis
Initially, careful palpation or feeling of the malleolus and surrounding area can indicate that a fracture may or may not be present.
Maximal tenderness on the bone may indicate a fracture, whereas if the area just forward or under the bone is more tender, this may indicate a ligament sprain.
An x-ray is the only way to determine for definite if a fracture is present.
Early x-rays may not clearly show this due to swelling and bleeding in the area.
If you suspect a fracture, then a second x-ray may be requested once the swelling has gone down.
Differential Diagnosis
There are many other conditions and injuries that can mimic a Pott’s Fracture in the absence of an obvious, sudden injury.
The following are examples of other ankle conditions:-
- Acute Compartment Syndrome .
- Lateral Ankle Ligament Tear.
- Deep Vein Thrombosis .
- Thrombophlebitis .
- Syndesmotic Disruption .
- Gout .
- Rheumatoid Arthritis .
- Talar Fracture .
Outcome Measures
There are many outcome measures available when assessing ankle fractures.
Some are designed to measure function limitation whilst others rely on patient reported outcome measures, which focus on patients reporting on their activities of daily living, pain, and other functional outcomes .
- Clinical Demerit Points .
- Maryland Foot Score .
- Walking speed .
- Time required to climb a set number of stairs .
- 36-item Short-Form Health Survey (SF-36) .
- Short Musculoskeletal Functional Assessment (SMFA) .
- Ankle-Fracture Outcome of Rehabilitation Measure (A-FORM) .
- Olerud and Molander (O&M) Questionnaire .
- Lower Extremity Functional Scale (LEFS) .
Investigations

Plain Skiagrams
Skiagrams in antero-posterior, lateral and mortise views are essential and are usually sufficient for diagnosis and management.
Mortise view is taken with leg in 15–20 degrees of internal rotation.
Several lines and angles have been mentioned to be seen on skiagrams to determine the integrity of the ankle joint.
They are:-
i) Tibiofibular line:-On the mortise view a line formed by subchondral bone of distal tibia and medial aspect of fibula should be continuous .
ii) Talocrural angle:-This is formed on mortise view by a line drawn parallel to the articular surface of distal tibia and one connecting the tips of both malleoli.
The angle is normally between 8 and 15 degrees .
iii) Talar tilt:-Lines drawn parallel to the articular surfaces of distal tibia and talus should be parallel .
iv) Medial clear space:-On mortise view the distance between the lateral border of medial malleolus and medial border of the talus is measured.
Normally this is equal to the superior clear space. A space of greater than 2 mm is abnormal and indicates lateral shift of the talus .
v) Syndesmotic integrity:-Fibula is posterior and lateral to tibia, so anterolateral part of tibia overlaps fibula.
On antero-posterior view this overlap should be less than 10 mm in syndesmotic injuries.
Tibiofibular or interosseous clear space should be less than 5 mm on antero-posterior view .
Stress views are used to confirm suspected ligamentous instability and compared with identical skiagrams of opposite side.
Arthrography is performed to evaluate the integrity of the joint capsule and ligaments .
It is seldom required. Tomography is helpful in evaluating complex fracture patterns and where the facilities for CT scan are not available.
Computed tomography is indicated in grossly comminuted fractures of the lower end of tibia where the fracture pattern is not clearly seen on plain skiagrams.
3-D reconstructions provide additional information and help in planning the reduction and fixation of fracture.
Osteochondral fractures and chronic ligamentous injuries are better seen on MRI. Arthroscopy of
the ankle is extremely useful for evaluating and managing osteochondral lesions of the talus .
Management
One of the most important components of rehabilitation following Pott’s fracture is that the patient rests sufficiently from any activity that increases their pain.
Activities which place large amounts of stress through the ankle should also be avoided, particularly excessive weight bearing activity such as running, jumping, standing, or walking.
Displaced Pott’s fractures where the anatomical relationship of the bones of the ankle has been disrupted need to be surgical fixation.
Post-operatively, protective boot, brace, or a plaster cast, and/or crutches are used for a number of weeks.
Fractures that are not displaced, treatment may involve a plaster cast immobilization and the use of crutches, followed by the use of a protective boot or brace for a number of weeks.
Patients with a Pott’s fracture should perform pain-free flexibility, strengthening, and balance exercises as part of their rehabilitation to ensure an optimal outcome.
The physiotherapist may utilize techniques such as massage and joint mobilization essential to ensure optimal range of movement and flexibility.
The aim of the massage is to fight the formation of heterotopic ossification.
This is the process by which bone tissue forms outside of the skeleton.
The treatment may also involve electrotherapy, taping and bracing, exercises to improve strength, flexibility and balance, and hydrotherapy.
Lengthening of the tendon Achilles is proved to be a treatment for complicated Pott’s fractures.
Lengthening or stretching of this tendon can be done by performing a passive dorsiflexion of the foot while the leg/knee is straight.
Physiotherapy treatment
Physiotherapy treatment is vital in all patients with a Pott’s fracture to hasten healing and ensure an optimal outcome. Treatment may comprise:-
- soft tissue massage .
- joint mobilization .
- dry needling .
- electrotherapy (e.g. ultrasound) .
- taping or bracing .
- the use of a protective boot or brace .
- the use of crutches .
- exercises to improve strength, flexibility and balance .


- hydrotherapy .
- education .
- activity modification .
- a graduated return to activity plan .
- footwear advice .
Other intervention for a Pott’s fracture
Despite appropriate physiotherapy management, some patients with a Pott’s fracture do not improve adequately and may require other intervention.
The treating physiotherapist or doctor can advise on the best course of management when this is the case.
This may include further investigations such as X-ray, CT scan, MRI or bone scan, periods of plaster cast immobilization or referraltoappropriate medical authorities who can advise on any intervention that may be appropriate to improve the Pott’s fracture.
Occasionally, patients with fractures that are initially managed without surgical intervention may require surgery to stabilize the fracture and a bone graft to aid fracture healing.
Exercises for a Pott’s fracture
The following exercises are commonly prescribed to patients with a Pott’s fracture following confirmation that the fracture has healed or that pain free mobilization can commence as directed by the surgeon.
You should discuss the suitability of these exercises with your physiotherapist prior to beginning them.
Generally, they should be performed 3 times daily and only provided they do not cause or increase symptoms.
Foot and Ankle Up and Down

Move your foot and ankle up and down as far as possible and comfortable without pain. Repeat 10 – 20 times provided there is no increase in symptoms.
Foot and Ankle In and Out

Move your foot and ankle in and out as far as possible and comfortable without pain . Repeat 10 – 20 times provided there is no increase in symptoms
Foot and Ankle Circles
Move your foot and ankle in a circle as large as possible and comfortable without pain .
Repeat 10 times in each direction provided there is no increase in symptoms. Other intervention for a Pott’s fracture
Despite appropriate physiotherapy management, some patients with a Pott’s fracture do not improve adequately and may require other intervention.
The treating physiotherapist or doctor can advise on the best course of management when this is the case.
This may include further investigations such as X-ray, CT scan, MRI or bone scan, periods of plaster cast immobilization or referral to
appropriate medical authorities who can advise on any intervention that may be appropriate to improve the Pott’s fracture.
Occasionally, patients with fractures that are initially managed without surgical intervention may require surgery to stabilize the fracture and a bone graft to aid fracture healing.
Physiotherapy products for a Pott’s fracture
Some of the most commonly recommended products by physiotherapists to hasten healing and speed recovery in patients with an ankle fracture include:
- Crutches.
- Protective Boots.
- Ankle Braces.
- Ankle Supports.
- Ice and Heat Packs.
- Wobble Boards (for rehabilitation).
- Dura Discs (for rehabilitation).
- Bosu Balls (for balance exercises).
- Resistance Band (for strengthening).
- Sports Tape (for protective taping).
Exercises
An ankle fracture exercise program should be the main component of your ankle rehabilitation following a fracture.
Exercises may include :-
- Exercises for ankle range of motion .
- Ankle strengthening exercises .
- Hip and knee exercises (to help improve walking ability) .
- Balance and proprioception exercises.
- Exercise to improve functional mobility and walking ability .
Post - operative pt management :-
Phase 1 (up to 6 week )
- PWB
- df to neutral
- control edema
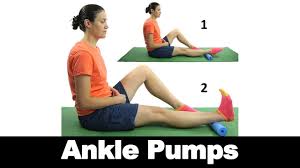
1) AROMS of ankle , subtalar joint , MT joint within pain tol.
ankle pumps
inv/env

2) calf streching, heel slides

3) elevation of edema
4) static quads and hams

5) 2-4 week , initial weight bearing as tolerate with cruches followed by PWB
Phase-2 (6 to 8 week)
Goals
- FWB involved LE
- control edema
- minimize complications
- maintain optimal bone and soft – tissue healing
- AROMS
- PROMS in restricted range
- heel slides
- calf streching
- ankle isometric
- grade 1,2 mobilization for ankle and sub talar joints
- leg circle ,leg press
- wall strech with KF and KE
- FWB walking , minisquat ,standing heel raise , one leg balance on floor
- wobble board exercise
Phase-3 (>8week)
Goals
- full ROMS
- restore gait on levels of surfaces , heel , stairs
Full return to function
- cnt phase2 exercise
- progrss to theraband exercise
- squat and launges exercise also wobber board exercise
- one leg standing exercise with eye open and eye closed
- stair climbing exercise
- Agility training
Complications
The commonest complication is nonunion. Most nonunions involve the medial malleolus.
These are often avulsion injuries that were initially treated conservatively and failed to unite because of residual displacement of the fracture, interposition of soft tissues or associated lateral instability resulting in shearing forces on the fracture from the pull of the deltoid ligament.
Treatment is with open reduction, internal fixation and bone grafting. Nonunion of the lateral or posterior malleolus is uncommon.
Malunion is more common and incongruity of the articular surface can alter the mechanics of the joint and
leadtopersistentsymptoms,degenerative changes, and loss of function of the joint.
A painful arthrosis after ankle fracture may result from severe cartilage damage at the time of injury, a malaligned and shortened lateral malleolus.
An arthrodesis is the treatment of choice for severe cartilage damage.
Marginal necrosis of skin edges after surgery occurs in about 3% of patients.
These problems can be decreased by avoiding surgery during the period of increased swelling, minimizing tourniquet time, careful handling of the soft tissues especially the skin edges, gentle retraction, use of implants appropriate for the size of the fracture fragments, wound closure without tension, appropriate drainage of the wound and avoiding constrictive dressings.
The use of posterior antiglide plates in fibular fractures has also been helpful in reducing the tension on the skin.
The risk of infection can be decreased with careful attention to the handling of the soft tissues and the technical aspects of internal fixation.
The infection rate in treating closed fractures with the current techniques of internal fixation is less than 2%.
Osteoarthritis can result from damage to the articular cartilage at the time of the injury from altered mechanics of the joint resulting from ligamentous instability or inadequate reduction of the fracture or both.
An ankle arthrodesis is the most dependable method of treatment for preven
tion of pain. Reflex sympathetic dystrophy may be a disturbing complication of ankle injuries.
Heterotopic bone may form between the distal tibia and fibula after injuries to the syndesmosis.
Ossification is usually seen at the level of the fibular fracture and often in association with the use of a syndesmotic screw.
Osteochondral (transchondral) fractures of the talus can occur after any type of injury to the ankle, including simple sprains.
Prognosis
In the most severe cases of a Pott’s fracture, patients usually make a full recovery with appropriate management. Return to activity or sport can usually take place in a number of weeks to months.

0Comments