Magnetic resonance imaging (MRI) is a topic that is delivered in a variety of different formats throughout medical school, therefore students and healthcare professionals alike may receive different standards of teaching. There are several different types, viewing planes, and a large range of associated pathologies to visualise.
These complexities may make students intimidated by MRI interpretation. Here, we provide a brief overview of MRI fundamentals, approach, and interpretation. Whilst we won’t be able to turn you into a radiologist, we may be able to help you look less confused when you next get quizzed by one.
Why do we need to use MRIs?
Generally, MRI is used less commonly than plain films and CT scans. They are often reserved for superior viewing of soft tissues. MRI is particularly helpful in patients with suspected neurological or musculoskeletal pathology, however, they can be used in many other specialities too. It takes slightly longer to acquire MR images and they are more expensive. MRI is contraindicated in patients who have ferromagnetic metal implants or foreign bodies.1 Consideration should be given to patients who are claustrophobic as well.
How do they work?
MRI machines work by exploiting the interaction of the magnetic field, hydrogen ions, and radiofrequency (RF) pulse. When you put a patient in a strong magnetic field, their hydrogen ions align in the direction of the magnetic field. Applying an RF pulse will change the direction of alignment of these hydrogen ions. When the RF pulse is turned off, these ions will attempt to realign with the magnetic field again and release a signal. The strength of this signal depends on the type of tissue (fat, muscle, water) that the hydrogen ion is in.
Using these principles, you can adjust the machine to detect signals of varying ranges and from varying planes of magnetisation – this is where the “weighted imaging” comes in. We can also tell the machine to disregard certain values of signals to “suppress” them when it comes to viewing the pictures – these are known as “fat suppression” sequences.
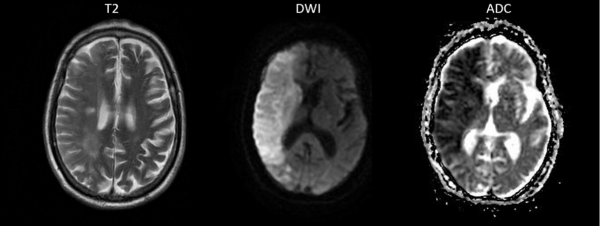
MRI can also be used as a dynamic imaging tool. For example, diffusion of water molecules can be studied with diffusion-weighted imaging (DWI), or macroscopic movement of blood can be studied, in the case of MR angiographic techniques.
MRI images and sequences
There are many factors that lead to the production of a final MR image. Different combinations of these will be useful for different clinical presentations, but here are some examples of common images and sequences:
- T1-weighted and T2-weighted imaging (T1WI and T2WI)
- DWI and ADC
- FLAIR
- STIR
and many others.
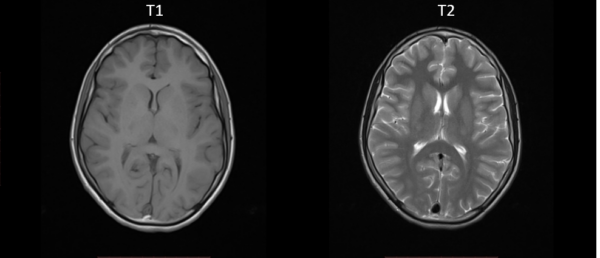
T1 and T2 weighted images
T1 and T2 images demonstrate different tissues based on the timing of the RF pulses. Between the two, the key differences you need to be aware of are:
- T1 – ONE tissue is bright: fat
- T2 – TWO tissues are bright: fat and water (WW2 – Water is White in T2)
- T1 is the most ‘anatomical’ image (Figure 1). Conversely, the cerebrospinal fluid (CSF) is bright in T2 due to its’ water content.
- T2 is generally the more commonly used, but T1 can be used as a reference for anatomical structures or to distinguish between fat vs. water bright signals.
Additional features of T1/T2 weighted images
Fat suppressed
The fat signal can be suppressed to enable a better view of pathology in and around anatomical structures – particularly oedema. This is useful in adrenal tumours or bone marrow pathology, where the image will appear homogenous with surrounding tissue due to fat content.
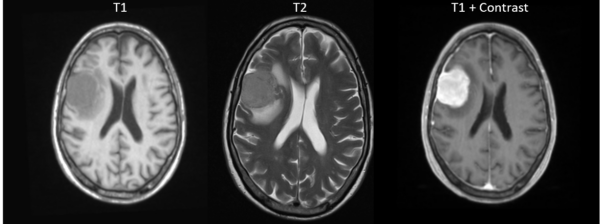
Gadolinium-enhanced
Gadolinium enhances vasculature (i.e. arteries) or pathologically-vascular tissues (e.g. intracranial metastases, meningiomas). This process involves injecting 5-15ml of contrast intravenously, with images taken shortly thereafter. Gadolinium appears bright in signal, allowing for detection of detailed abnormalities (e.g. intracranial pathologies). Typical intracranial abscesses have a “ring-enhancement” pattern, while metastases enhance homogeneously. Meningiomas will have a homogenous enhancement after the contrast, but will also have a “dural tail,” meaning the lesion appears continuous with the dura.
Inversion recovery (IR) sequences
These types of images are manipulations of T1 and T2. They nullify certain tissue types based on their inversion timings, thereby stopping tissues such as fat and CSF from appearing as bright signals. This is helpful to identify pathological signals. The two main types are discussed below.
Short tau inversion recovery (STIR)
STIR is based on a T2 image, but the image is manipulated in a way that results in fat (and any other materials with similar signals) being nullified. Unlike fat-suppressed images, however, STIR can not be used with gadolinium contrast.4 As previously discussed, fat can make the interpretation of oedematous areas and bone marrow difficult. Figure 3 shows how this nullified fat signal can assist with the identification of oedema due to fractures.

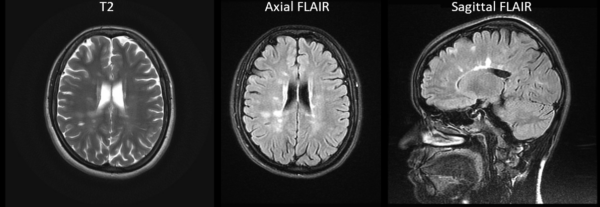
Fluid attenuated inversion recovery (FLAIR)
FLAIR is also similar to T2, however, the CSF signal is nullified. This is particularly useful for evaluating structures in the central nervous system (CNS), including the periventricular areas, sulci, and gyri. For example, FLAIR can be used to identify plaques in multiple sclerosis, subtle oedema after a stroke, and pathology in other conditions whereby CSF may interfere with interpretation (Figure 4).1
Diffusion-weighted imaging (DWI) and apparent diffusion coefficient (ADC)
DWI is an imaging modality that combines T2 images with the diffusion of water. With DWI scans, ischaemia can be visualised within minutes of it occurring (Figure 5). This is because DWI has a high sensitivity for water diffusion, thereby detecting the physiological changes that happen immediately after a stroke.
A systematic approach to MRI interpretation
Verify details
Begin by verifying the following details:
- Patient details (i.e. name, date of birth, hospital number)
- Image details (i.e. date, type)
- Make sure it is the most recent image for the correct patient
- Look for previous cross-sectional imaging (if available)
Look at the T2 weighted images
Inspect the T2 weighted images:
- Look at each available plane (axial, coronal, sagittal)
- Check for abnormal MRI signals
- Work through the anatomy of the areas you are looking at to make sure nothing is missed/abnormal
- Comparing both sides of an image (if possible) can reveal clear areas of abnormal signalling
- Shape, size, location, and intensity of the signal
Compare different MRI image sequences
Compare the available MRI image sequences to help differentiate pathology:
- Comparing fat sensitive images (e.g. T1) vs water-sensitive images (e.g. T2 or STIR) can help differentiate pathologies such as ischaemia and inflammation.
- Post-contrast enhancement is useful for vascular pathology or pathologically-vascular tissue.
- Learn why each image type is used – this will enable you to know what you are looking for (e.g. for MR brain it’s useful to look at T2, then FLAIR, then DWI/ADC, as this will help distinguish between most differentials).
Compare against other imaging modalities
Compare the MRI images to other imaging modalities (e.g. ultrasound, CT, plain film):
- Can you view the pathology on other imaging modalities?
- Plain films can be particularly useful when assessing musculoskeletal pathology.
Compare against previous images
Compare the current MRI images to previous MRI scans if available:
- Are the abnormal signals new or old?
- Are there any changes in the size/shape/brightness of the abnormal signals?
Consider the clinical context
Finally, place your findings in context with the clinical presentation in order to ascertain a radiological diagnosis:
- Are the symptoms acute or chronic?
- How unwell is the patient?
- Does the imaged pathology correlate with the presenting symptoms?
Summary
In this article, we have outlined the basics of different types of MRI, along with key examples. A lot has been covered, and a lot has not, but this will give you a good understanding of the fundamentals of MRIs.
The key points are as follows:
- MRIs are a superior imaging modality for viewing soft tissues.
- T1 and T2 weighted images represent the core types of MR images.
- T1 and T2 images may be adjusted: fat-suppressed, gadolinium-enhanced and inversion recovery.
- The different sequences tell you what is in the lesion and how it is behaving. Using these features, the location of the lesion, and the clinical history, we can make a diagnosis.
- Anatomy, as with all scans, is key. MRIs produce a very clear view of structures, therefore strong anatomical knowledge is particularly helpful.
- Spend time looking at normal scans. The more you become familiar with what is normal, the easier it is to see when things are abnormal.
- Always compare both sides of the scan – pathology is rarely bilateral.
- Be methodical!
References
- Bitar, R. et al. MR pulse sequences: What every radiologist wants to know but is afraid to ask. Published in 2006. Available from: [LINK]
- Dr Hidayatullah Hamidi. Normal brain MR shows differences between T1 and T2 images. Licence: [CC BY-SA].
- Andrew Murphy, et al. MRI sequences (overview). Radiopaedia.org, the wiki-based collaborative Radiology resource. [Internet] (Accessed: 21st March 2020). Available from: [LINK]
- Assoc Prof Frank Gaillard. Meningioma shown more clearly by gadolinium contrast with a dural tail. Licence: [CC BY-SA]. Available from: [LINK]
- Dr Dalia Ibrahim. STIR shows marrow oedema in L1 vertebra, indicative of a fracture. Licence: [CC BY-SA].
- Dr Mahmoud Rashed. Multiple sclerotic plaques in periventricular regions and corpus callosum. Licence: [CC BY-SA].
- Dr Bahman Rasuli. Recent right-sided ischaemic stroke. Licence: [CC BY-SA].



0 Comments