Allergic disease is determined by the complex interplay of environmental and genetic factors. It affects around 20% of the world population making it a growing health and clinical concern. Even though the generation of the allergic response is quite well understood, the factors contributing to the development of allergies are still not clear.
The genetic basis of allergies
Our bodies protect us from dangerous factors via activation of the immune system. Immunoglobulin E (IgE) are antibodies that are produced by the immune system. Allergies and the atopic reaction associated with them are mediated by IgE. Atopy is the genetic predisposition to develop allergic conditions such as asthma, allergic rhinitis and atopic dermatitis. IgE plays a key role in the spectrum of reactions to foreign bodies; thus it protects us by eliminating the potential danger.
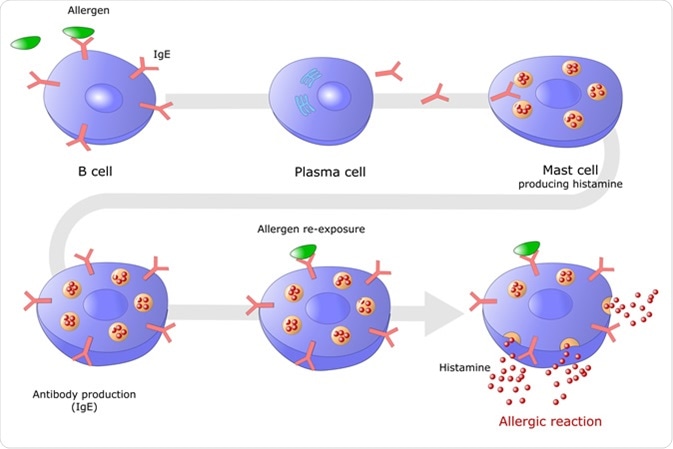
A discovery made in 2008 indicated that the FCER1A gene is responsible for encoding an alpha chain of high-affinity IgE receptors. Certain variations of this gene cause the production of IgE antibodies and an elevated level of these antibodies is associated with an allergic response.
Evidence for the genetic basis of allergies comes from studies looking at the familial aggregation of allergies and asthma. Research has shown that the risk of developing asthma or any other allergies is higher if the person has a family history of asthma or allergies.
Now more than ever research is focusing on the genetic basis of atopic configuration due to the increasing incidence of IgE atopy and the fact that most common treatment options are only focused on relieving symptoms.
The genetics of food allergy
The increased amount of IgE in people who have allergies can lead to their bodies rejecting seemingly harmless things such as peanut butter and milk. Food allergies affect 5-8% of children and 1-5% of adults worldwide.
The current knowledge about the biological mechanisms of food allergy process is still not clear. It is generally accepted that both genetic and environmental factors, determine food allergies.
Several genes have been linked to food allergies. Family studies support this by showing that family history increases the risk of having a food allergy. A rather unbiased approach to linking genetics with food allergies is the genome-wide approach. This technique examines the association between the genotype of a common variant and the disease susceptibility across the entire genome. Studies of this kind have illustrated the role of HLA gene in allergies.
The field has shifted towards considering the complex gene-environment interaction in the susceptibility of someone developing an allergy. However, due to the small sample sizes and population differences, the results are still inconsistent and not enough to validate the relationship between certain genes and allergies.The advancement in the field of genomics, the study of the entirety of the organism’s genes, called the genome, and the use of genome information has spurred incredible interest in this area and laying the foundation for prediction, prevention and treatment of food allergies.
Candidate Gene Evaluation Method
One of the ways to genetically test a predisposition to allergies is via candidate gene evaluation. This method involves using a large sample of people to test the association between a gene variant and a certain feature or disease such as allergies.
Asthma studies have found a relationship between developing the disease and the following genes: cytokine genes, cytokine receptor genes, HLA genes and CD14 gene.
A very big limitation in these studies and a problem with genetic tests, in general, is the difficulty to replicate studies with a different sample of people and still getting significantly meaningful results. Moreover, results should be looked at with some caution due to the likelihood of them being caused by a statistical error.
Also, the range of candidate genes linked to a certain phenotype, that is the observable characteristics resulting from the interaction of its genotype with the environment, is rather small if you compare it to the total number of genomes.
By taking a DNA test you can find out your body’s sensitivity to foods and how your genetic predisposition impacts your ability to digest certain foods. Using this information you can adjust your diet and lead a healthier lifestyle.
How accurate are these genetic tests?
There is growing popularity in the commercially available DNA tests. Only a mouse click separates you from finding out information related to ancestry, health, disease predisposition and so forth. However, issues related to the scientific reliability of the results provided by these tests have been raised.
Segregation analysis has been used to study family heritability to determine the likelihood of allergies or any disease development. This is an analytical method which aims to fit observed data under an expected curve of data points. This means that the way genetic tests work is by taking an individual sample and comparing it to a preselected pool of data and inferring a certain level of similarity in the genes. The larger the sample, the more reliable the results are. But some questions remain: how big a sample should be and how can you generalize across the whole world?
Though genetic tests have given hope to many scientists in their pursuit of uncovering the causes of many diseases, interpretation of the results from these tests should be done with caution. Simply because a test tells you that you are allergic to peanut butter does not necessarily guarantee that this is 100% true. By no means is this a factor that should stop people from using genetic tests to uncover their potential predisposition to allergies. It simply implicates that other tests should also be taken to support the genetic results before you spend your whole life avoiding peanut butter.
References
- Li, J., Maggadottir, S. & Hakonarson, H. (2017). Are genetic tests informative in predicting food allergy? https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5407010/
- Hong, X., Tsai, H. & Wang, X. (2010). Genetics of Food allergy. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2892276/
- Steinke, J., Rich, S. & Borish, L. (2008). Genetics of allergic disease. https://www.sciencedirect.com/science/article/pii/S0091674907014285
- Zhoua, J et al. (2011). Association of polymorphisms in the promoter region of FCER1A gene with atopic dermatitis, chronic uticaria, asthma, and serum immunoglobulin E levels in a Han Chinese population. https://www.ncbi.nlm.nih.gov/pubmed/22222815


0 Comments