Artificial insemination (AI) or intrauterine insemination refers to a technique that is used to help infertile couples conceive.
AI is based on the insertion of sperm from a male, who is either the patient's partner or a donor, into a woman’s womb, to facilitate fertilization of the woman’s ovum. The purpose of AI is to increase the number of sperm within the fallopian tube in order to increase the odds that conception will occur.
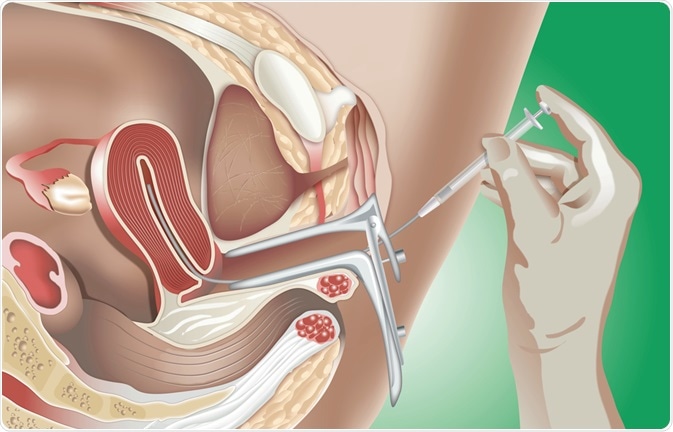
Image Credit: alexonline / Shutterstock.com
AI is often used by couples whose infertility is due to mild male factor dysfunction; however, it is also used for unexplained mild infertility. To this end, donor insemination is used when the male factor is affected and natural conception by the male partner nearly impossible, as is the case when there is azoospermia or severe oligospermia. In some cases, AI is preferred when the offspring may be liable to inborn diseases carried on the Y-chromosome.
Criteria
Though specific criteria may vary from country to country, in general, six cycles of AI are offered for the following indications:
- Cervical mucus antibodies or other cervical factors that cause the environment to be hostile to fertilization by normal intercourse
- Mild endometriosis
- Mild to moderate male factor infertility
- Unexplained infertility
- Physical or psychological factors make normal intercourse impossible
- Use of sperm which was collected and frozen for later use because of chemotherapy or radiation therapy
- A high possibility of sexually-transmitted disease that makes it necessary to avoid natural conception
- Same-sex couples who desire to conceive using donor sperm
Benefits
AI is more useful in women who are not over the age of 35, as oocyte quality tends to drop after the age of 35, thus making fertilization less likely.
Costs
While not as expensive as in vitro fertilization, AI can cost thousands of dollars per cycle when performed at private treatment centers.
Procedure
Before an AI, the woman’s internal organs are evaluated to ensure that the tubes are healthy and free of adhesions. Fallopian tubes that are free of adhesions allow the sperms to rapidly and freely move through them to achieve fertilization. The inspection of a woman's internal organs may be conducted by laparoscopy, hysterosalpingography, or hysterosonography with contrast.
AI may be performed following natural ovulation or after inducing ovulation with ovary-stimulating medication. First, ovulation is confirmed by ultrasound, a blood test, or home testing kits. The male partner is then asked to provide a semen sample. The semen sample is processed to concentrate the motile sperm, and the final preparation is inserted through a fine catheter into the uterine cavity.
If donor sperm is used, frozen sperm, which is typically acquired from a sperm bank, is used. Careful counseling is needed beforehand to ensure that the offspring is accepted by both parents. The sperm provided by the donor will be screened for infections such as hepatitis B, hepatitis C, and HIV, as these infections could be carried through the semen. Some genetically transmissible disorders will also be tested for. In addition, sperm from a physically compatible donor may be used by the bank on request.
Adverse effects
Pain is rare, though mild abdominal cramps or discomfort may be present because of the passage of the catheter. Rarely, some women have can be allergic to the ovarian stimulation medication. The multiple pregnancy rate is slightly increased when AI is employed.
Success
The conception rate following AI is estimated to be more than 50% when six cycles are used. Overall, the success rate of AI varies based on:
- The age of the woman, as the success rate per cycle is just under 16% for women under 35 years and very low for women above the age of 44.
- Sperm count
- Sperm quality
- Fresh versus frozen and thawed sperm
- Precise identification of the ovulation period


0 Comments