University of Missouri scientists are partnering with Harvard and Georgia Tech to create a new diabetes treatment that involves transplanting insulin-producing pancreatic cells
Type 1 diabetes is estimated to affect around 1.8 million Americans. Although type 1 diabetes often develops in childhood or adolescence, it can occur in adulthood.
Despite active research, type 1 diabetes has no cure. Treatment methods include taking insulin, monitoring your diet, managing blood sugar levels, and exercising regularly. Scientists have also recently discovered a new treatment method that holds promise.
A group of researchers from the University of Missouri, Georgia Institute of Technology, and Harvard University has proved the successful use of a novel Type 1 diabetes treatment in a large animal model in a new study published in Science Advances on May 13th. Their method includes transferring insulin-producing pancreas cells, known as pancreatic islets, from a donor to a recipient without the need for long-term immunosuppressive medicines.
According to Haval Shirwan, a professor of child health and molecular microbiology and immunology at the MU School of Medicine and one of the study’s primary authors, people with Type 1 diabetes’ immune system may malfunction, leading it to target itself.
“The immune system is a tightly controlled defense mechanism that ensures the well-being of individuals in an environment full of infections,” Shirwan said. “Type 1 diabetes develops when the immune system misidentifies the insulin-producing cells in the pancreas as infections and destroys them. Normally, once a perceived danger or threat is eliminated, the immune system’s command-and-control mechanism kicks in to eliminate any rogue cells. However, if this mechanism fails, diseases such as Type 1 diabetes can manifest.”
Diabetes impairs the body’s ability to produce or utilize insulin, a hormone that aids in the regulation of blood sugar metabolism. People with Type 1 diabetes are unable to manage their blood sugar levels because they do not produce insulin. This lack of control may result in life-threatening problems including heart disease, kidney damage, and vision loss.
Shirwan and Esma Yolcu, a professor of child health and molecular microbiology and immunology at the MU School of Medicine, have spent the last two decades targeting an apoptosis mechanism that prevents “rogue” immune cells from causing diabetes or rejection of transplanted pancreatic islets by attaching a molecule called FasL to the islets’ surface.
“A type of apoptosis occurs when a molecule called FasL interacts with another molecule called Fas on rogue immune cells, and it causes them to die,” said Yolcu, one of the study’s first authors. “Therefore, our team pioneered a technology that enabled the production of a novel form of FasL and its presentation on transplanted pancreatic islet cells or microgels to prevent being rejected by rogue cells. Following insulin-producing pancreatic islet cell transplantation, rogue cells mobilize to the graft for destruction but are eliminated by FasL engaging Fas on their surface.”

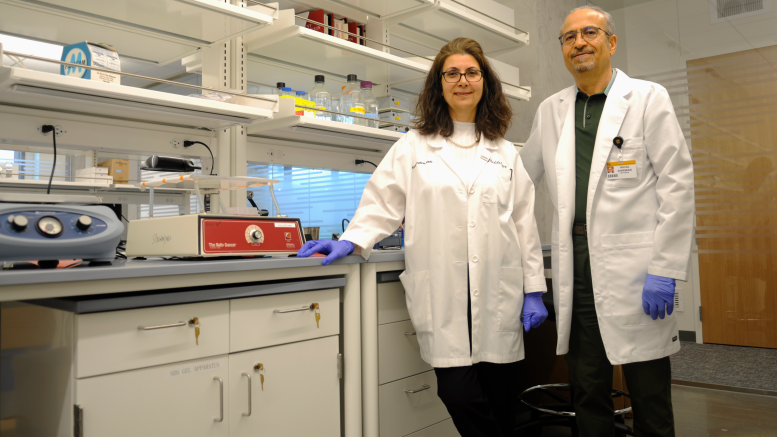
Haval Shirwan and Esma Yolcu work in their lab at the Roy Blunt NextGen Precision Health building. Credit: University of Missouri
One advantage of this new method is the opportunity to potentially forgo a lifetime of taking immunosuppressive drugs, which counteract the immune system’s ability to seek and destroy a foreign object when introduced into the body, such as an organ, or in this case, cell, transplant.
“The major problem with immunosuppressive drugs is that they are not specific, so they can have a lot of adverse effects, such as high instances of developing cancer,” Shirwan said. “So, using our technology, we found a way that we can modulate or train the immune system to accept, and not reject, these transplanted cells.”
Their method utilizes technology included in a U.S. patent filed by the University of Louisville and Georgia Tech and has since been licensed by a commercial company with plans to pursue FDA approval for human testing. To develop the commercial product, the MU researchers collaborated with Andres García and the team at Georgia Tech to attach FasL to the surface of microgels with proof of efficacy in a small animal model. Then, they joined with Jim Markmann and Ji Lei from Harvard to assess the efficacy of the FasL-microgel technology in a large animal model, which is published in this study.
Haval Shirwan looks at a sample through a microscope in his lab at the Roy Blunt NextGen Precision Health building. Credit: University of Missouri
Incorporating the power of NextGen
This study represents a significant milestone in the process of bench-to-bedside research, or how laboratory results are directly incorporated into use by patients in order to help treat different diseases and disorders, a hallmark of MU’s most ambitious research initiative, the NextGen Precision Health initiative.
Highlighting the promise of personalized health care and the impact of large-scale interdisciplinary collaboration, the NextGen Precision Health initiative is bringing together innovators like Shirwan and Yolcu from across MU and the UM System’s three other research universities in pursuit of life-changing precision health advancements. It’s a collaborative effort to leverage the research strengths of MU toward a better future for the health of Missourians and beyond. The Roy Blunt NextGen Precision Health building at MU anchors the overall initiative and expands collaboration between researchers, clinicians, and industry partners in the state-of-the-art research facility.
“I think by being at the right institution with access to a great facility like the Roy Blunt NextGen Precision Health building, will allow us to build on our existing findings and take the necessary steps to further our research, and make the necessary improvements, faster,” Yolcu said.
Shirwan and Yolcu, who joined the faculty at MU in the spring of 2020, are part of the first group of researchers to begin working in the NextGen Precision Health building, and after working at MU for nearly two years they are now among the first researchers from NextGen to have a research paper accepted and published in a high-impact, peer-reviewed academic journal.
Reference: “FasL microgels induce immune acceptance of islet allografts in nonhuman primates” by Ji Lei, María M. Coronel, Esma S. Yolcu, Hongping Deng, Orlando Grimany-Nuno, Michael D. Hunckler, Vahap Ulker, Zhihong Yang, Kang M. Lee, Alexander Zhang, Hao Luo, Cole W. Peters, Zhongliang Zou, Tao Chen, Zhenjuan Wang, Colleen S. McCoy, Ivy A. Rosales, James F. Markmann, Haval Shirwan and Andrés J. García, 13 May 2022, Science Advances.
DOI: 10.1126/sciadv.abm9881
Funding was provided by grants from the Juvenile Diabetes Research Foundation (2-SRA-2016-271-S-B) and the National Institutes of Health (U01 AI132817) as well as a Juvenile Diabetes Research Foundation Post-Doctoral Fellowship and a National Science Foundation Graduate Research Fellowship. The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding agencies.
The study’s authors would also like to acknowledge Jessica Weaver, Lisa Kojima, Haley Tector, Kevin Deng, Rudy Matheson, and Nikolaos Serifis for their technical contributions.
Potential conflicts of interest are also noted. Three of the study’s authors, García, Shirwan, and Yolcu, are inventors on a U.S. patent application filed by the University of Louisville and the Georgia Tech Research Corporation (16/492441, filed Feb. 13, 2020). In addition, García and Shirwan are co-founders of iTolerance, and García, Shirwan, and Markmann serve on the scientific advisory board for



0 Comments